Between 10% and 30% of people with untreated obstructive sleep apnea experience headaches after waking up in the morning. Sleep apnea headaches are typically frequent, occuring on most days of the week and can last up to several hours. Proper treatment for obstructive sleep apnea can help reduce the risk of waking up with a headache.
Can Sleep Apnea Cause Headaches?
Sleep apnea can cause headaches, but doctors don’t fully understand why. It’s believed that headaches are a result of changes in the body caused by the repeated disruptions in breathing that occur during sleep in people with obstructive sleep apnea (OSA).
Nighttime breathing disruptions in people with OSA can trigger several changes that may contribute to morning headaches. When a person’s breathing is disrupted, it decreases the level of oxygen in their blood and increases carbon dioxide. Changes in these blood gasses cause blood vessels to dilate, or widen, and increase pressure within the skull.
Experts believe that poor sleep quality may also contribute to sleep apnea headaches. People with obstructive sleep apnea often wake up multiple times each night to resume breathing. These frequent awakenings decrease the quality of sleep and may trigger or exacerbate headaches and migraines.
What Does a Sleep Apnea Headache Feel Like?
A sleep apnea headache typically feels like squeezing on both sides of the front of the head. Unlike with other types of headaches, a person typically does not feel nauseous, nor sensitive to light or sound.
Other Types of Headaches from Sleep Apnea
In addition to sleep apnea headaches, other types of headaches have been studied for potential links to obstructive sleep apnea.
Sleep Apnea and Migraines
Although sleep apnea itself is not thought to cause migraines, they can be triggered by a lack of sleep. Because sleep disorders like OSA can affect the quality of sleep, untreated OSA could make migraines worse.
Migraines are severe, throbbing headaches usually accompanied by nausea and sensitivity to light or sound. Migraines are common, affecting 12% to 15% of people in the United States. They are typically felt on one side of the head but can also be felt on both sides or all over the head. Migraines may last from around 4 to 72 hours.
In addition to poor quality sleep, other possible triggers for migraines include stress, hormonal changes, bright lights, loud noises, strong smells, sudden changes in temperature or weather, physical activity, and certain foods and medicines.
Sleep Apnea and Tension Headaches
Some studies have found an association between obstructive sleep apnea and tension headaches, while others have not. However, lack of sleep and other physical effects of obstructive sleep apnea could trigger tension headaches.
Tension headaches happen when muscles of the neck, face, and scalp become tense. These headaches are usually mild to moderate, do not throb, and are felt on both sides of the head. People often describe the pain as an elastic band squeezing the head.
Stress, anxiety, and depression are common triggers for tension headaches. Head and neck movements, or holding the head and neck in one position for too long, may also trigger tension headaches. Pain from tension headaches may last from 30 minutes to 7 days.
Sleep Apnea and Cluster Headaches
While there appears to be a connection between cluster headaches and obstructive sleep apnea, experts believe that this relation is likely indirect. Cluster headaches commonly occur during sleep and frequently cause a person to wake up.
Cluster headaches are not very common, affecting less than 1% of people. Cluster headaches feel like a sharp or stabbing headache felt around one eye or on one side of the head. They may also cause eyelid drooping, tear production, and nasal congestion on the affected side of the head.
Cluster headaches can last for 15 minutes or up to 3 hours and can occur every other day or up to 8 times a day. Cluster headaches may be triggered by drinking alcohol, smoking tobacco, high altitudes, bright light, too much physical activity, certain medicines, certain foods, and heat, among other things.
How to Get Rid of Sleep Apnea Headaches
Sleep apnea headaches may go away once a person receives treatment for obstructive sleep apnea. There are a variety of treatment methods used to reduce the effects of OSA, including positive airway pressure (PAP) therapy, lifestyle changes, oral appliances, and surgery.
If you are concerned that morning headaches may be related to sleep apnea, it’s important to talk with your doctor. A doctor can diagnose obstructive sleep apnea and rule out other potential causes of headaches. In some cases, a doctor may recommend medications to relieve discomfort from headaches.
PAP therapy
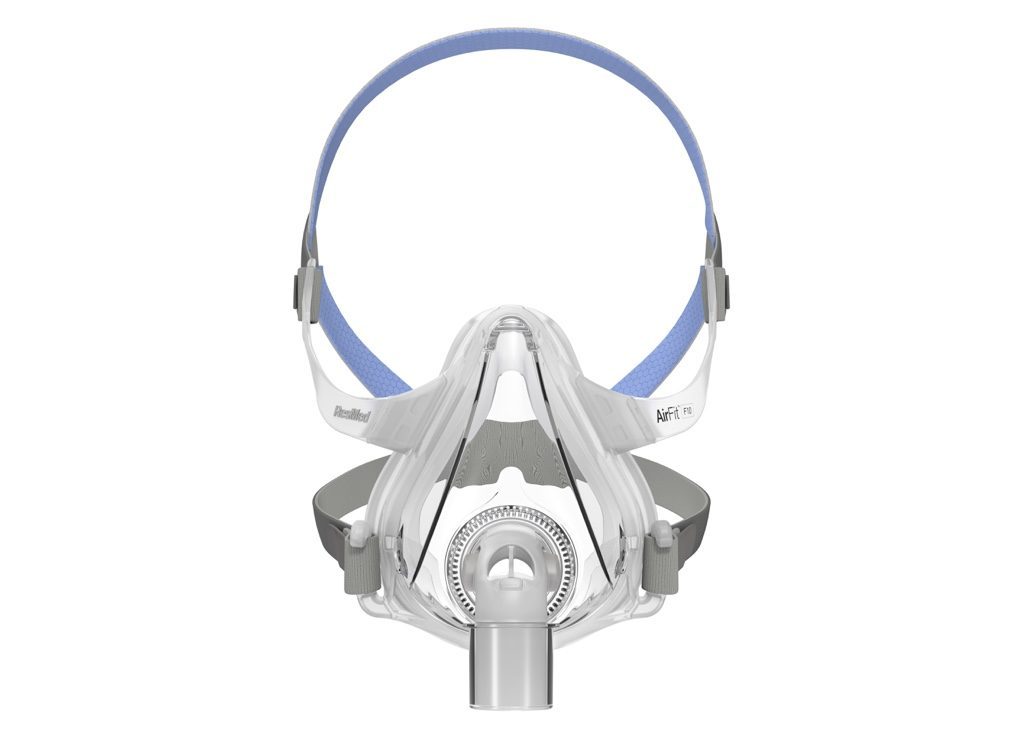
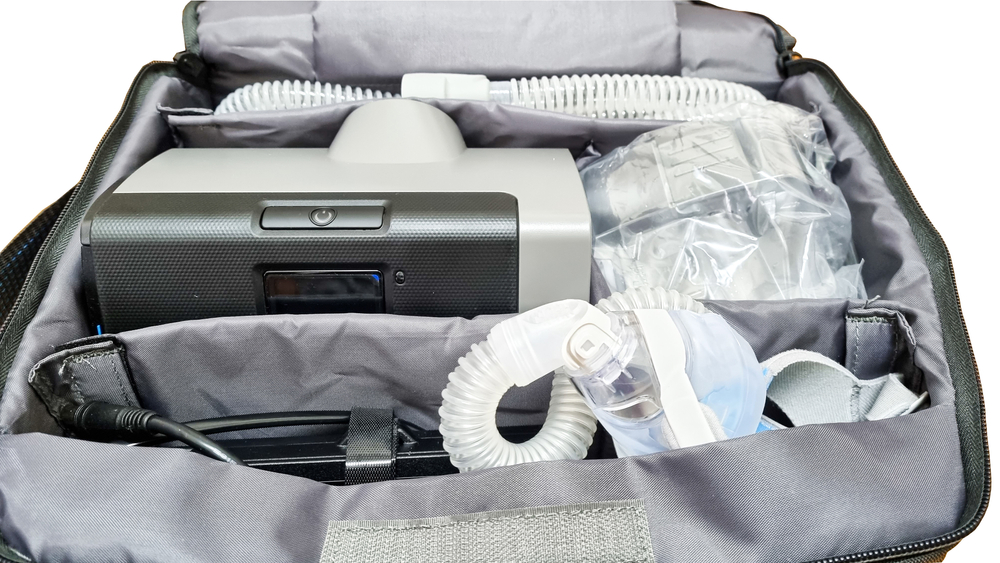
PAP therapy is the primary treatment used to reduce the signs and symptoms of obstructive sleep apnea. This treatment uses a machine to push filtered, pressurized air that prevents the airway from collapsing or becoming blocked during sleep.
There are several types of PAP machines. Continuous positive airway pressure (CPAP) is a common form of PAP therapy that delivers a steady stream of air each time a person inhales or exhales. Other PAP types deliver alternating or varied air pressures.
Lifestyle Changes
Exercise, changing sleep position, and reducing or avoiding alcohol and sedative medicines are all lifestyle changes that can help reduce the symptoms of OSA. Doctors may also recommend weight loss for people with obesity.
For some people, the symptoms of obstructive sleep apnea get worse when they sleep on their backs. If this is the case, a person can try sleeping on their side instead.
Other Treatments for Obstructive Sleep Apnea
Several other treatments are available for people in whom PAP therapy and lifestyle changes aren’t able to resolve obstructive sleep apnea.
- Oral appliances: Several oral appliances can be worn in the mouth at night that can reduce breathing disruptions during sleep, including mandibular advancement devices and tongue-retaining devices.
- Surgery: Surgery may be recommended for some people with OSA. It often is considered when other treatment options do not work and a person has severe OSA. Surgery may entail removing extra tissue or addressing structures in the mouth and throat that contribute to symptoms.
- Nerve stimulation: Hypoglossal nerve stimulation is a treatment for obstructive sleep apnea in which a device is surgically placed in the body. Upon activation, the device stimulates nerves in the tongue that help to keep the airway open during sleep.