A well-chosen CPAP mask doesn’t just fit your face—it fits your sleep style, your breathing needs, and your long-term comfort. For CPAP therapy to be effective, the mask must not only fit properly but also feel comfortable enough for consistent, nightly use.
Your doctor will guide you in selecting a CPAP machine and mask based on your diagnosis, but with over 9,000 possible mask combinations and customizable features, the process can feel overwhelming. Fortunately, understanding the different types of CPAP masks and knowing what to look for can make it easier to find the right fit for your needs.
Types of CPAP Masks
Finding the best CPAP mask is often a significant factor for determining how successful CPAP therapy will be in treating your obstructive sleep apnea. The right mask ensures that the machine delivers pressurized air effectively to keep your airway open throughout the night. Depending on whether you primarily breathe through your nose or mouth, different styles may offer better comfort and seal.
The three most common CPAP mask styles are:
- Nasal masks
- Nasal pillow masks
- Full-face (oronasal) masks
Nasal and oronasal masks are the most widely used masks for CPAP therapy. In particular, some experts may recommend a person try out a nasal mask first and then try other mask options if they're having problems with the fit or results.
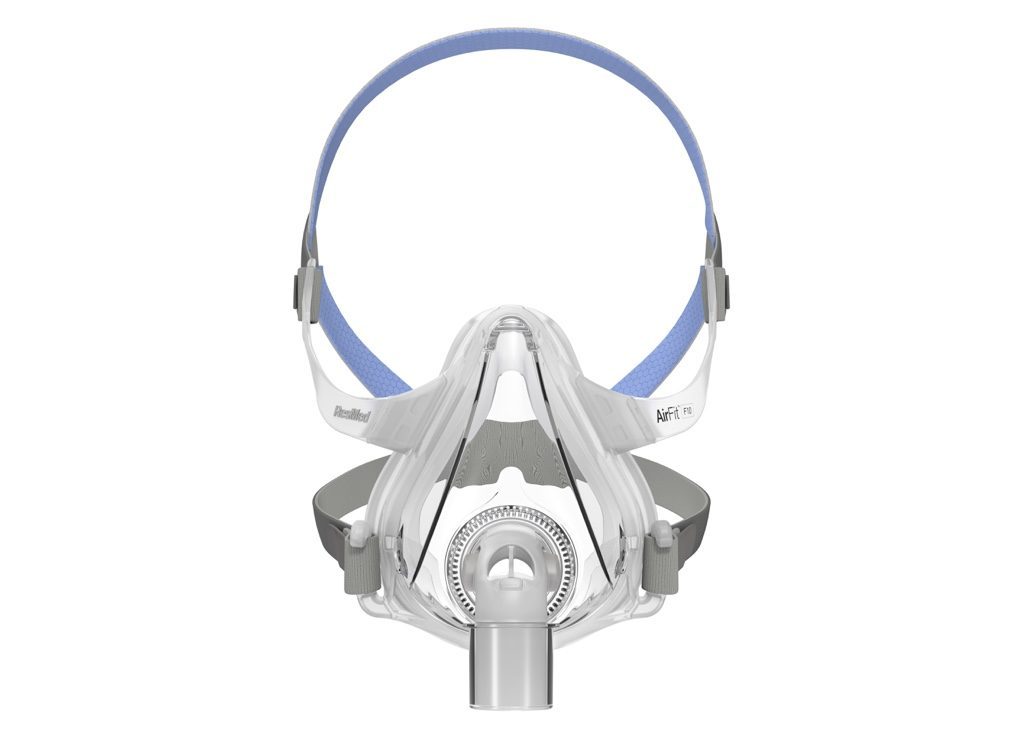
Full-Face (Oronasal) Masks
Full-face CPAP masks cover both the nose and mouth, making them ideal for users who breathe through their mouth while sleeping. They’re also commonly prescribed for people with high-pressure needs or who experience frequent nasal blockages.
Best for:
- Mouth breathers
- People with nasal obstructions or chronic allergies
- Individuals who require higher pressure settings
- Back sleepers who don’t mind a bit more facial coverage
- People who experience “mouth leaks,” which occur when the pressurized air from the CPAP machines escapes through the mouth
Not ideal for:
- Active sleepers who move around a lot
- People prone to claustrophobia
- Side sleepers who may experience leaks due to mask bulk
- Users with facial hair that could interfere with the seal
Nasal Masks
Nasal masks are designed to deliver pressurized air through the nose. A frame holds a flexible silicone cushion which fits around the perimeter of the nose, including the nasal bridge and above the upper lip. Nasal masks are secured to the face with a strap that attaches behind the head.
Best for:
- People who breathe through their nose while sleeping
- Those who move around during sleep (some nasal masks are designed to stay secure with movement)
- Individuals who find full-face masks too bulky
- Sleepers needing higher pressure settings without a full-face mask
Not ideal for:
- Mouth breathers (unless paired with a chin strap)
- People with nasal congestion or sinus issues
- Those who find pressure on the bridge of the nose uncomfortable
- Individuals with mustaches
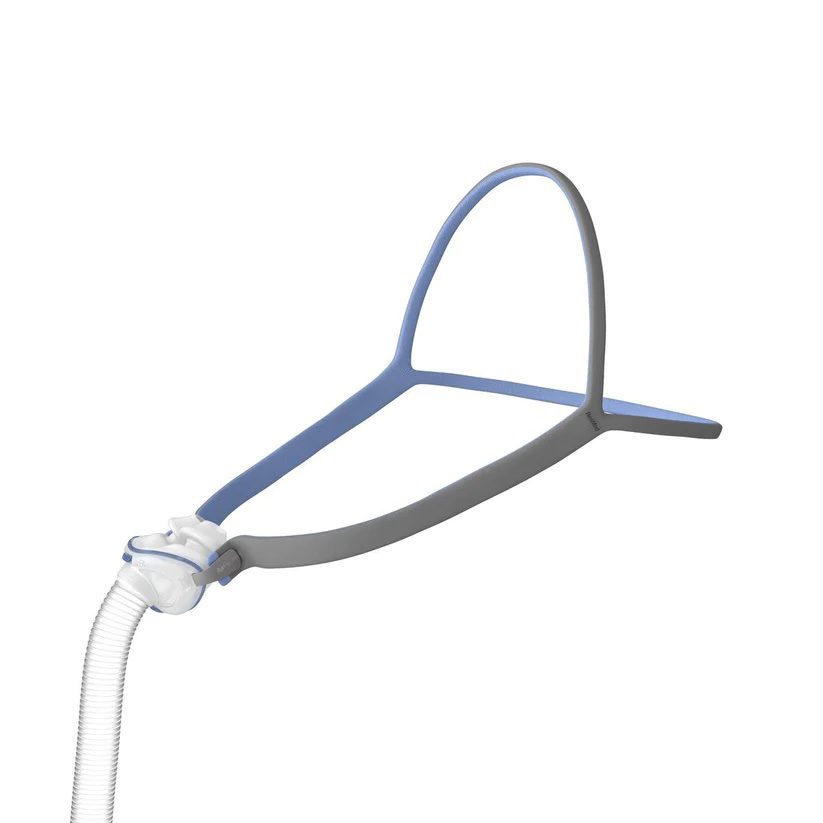
Nasal Pillows
Nasal pillow CPAP masks are small, lightweight interfaces that seal directly at the nostrils with soft, flexible pillows. They have minimal contact with the face and are a popular choice for those who prioritize a lightweight, low-profile design.
Best for:
- People who feel claustrophobic in larger masks
- Side or stomach sleepers who need minimal facial contact
- Individuals with facial hair (less surface area means a better seal)
- Users who wear glasses or read or watch TV before bed
Not ideal for:
- High-pressure CPAP users (pillows may be less effective at sealing under high pressure)
- Mouth breathers who don't want to use a chin strap
- Those with frequent nasal congestion or allergies
Hybrid Masks
Lastly, hybrid CPAP masks combine features of both full-face and nasal pillow masks, typically covering the mouth like a full-face mask while using soft nasal inserts or pillows instead of a traditional nasal cushion. This unique design allows for effective therapy with a lower profile and less bulk, which many users find more comfortable.
Hybrid masks can be a good option for people who breathe through their mouth but dislike the bulkiness or claustrophobic feel of standard full-face masks. They’re also useful for those with facial hair or other fit challenges that make traditional masks uncomfortable or prone to leaks.
However, hybrid masks may require more precise adjustment to ensure a proper seal and may not be ideal for users who move around a lot during sleep.
Finding the Right CPAP Mask for You
Choosing the right CPAP mask is a key step toward long-term comfort and successful therapy. While your doctor or sleep specialist can offer helpful guidance, asking yourself a few personal questions can help narrow down your options:
- Do you have facial hair? Facial hair can interfere with the seal of certain mask types, especially nasal and full-face masks.
- Do you mostly breathe through your mouth while sleeping? Mouth breathers may benefit more from full-face masks or chin straps paired with nasal masks.
- Are you an “active sleeper,” with frequent changes in body position during the night? Some mask styles, like nasal pillows or compact nasal masks, offer more freedom of movement.
- Are you claustrophobic? Lightweight and minimalist designs like nasal pillow masks may feel less restrictive.
- What's your preferred sleeping position? Side and stomach sleepers often prefer low-profile masks, while back sleepers have more flexibility in mask choice.
Once you’ve considered your sleeping habits and preferences, look closely at the features of each CPAP mask:
- Design: The mask’s shape and coverage—whether it sits under the nose, over the nose, or covers the mouth and nose—affect comfort and suitability for different sleepers.
- Adjustability: Masks with multiple adjustment points offer a more customizable fit, which helps prevent leaks and pressure marks.
- Material: The softness and breathability of mask materials, such as silicone, gel, or memory foam, can greatly affect comfort, especially for those with sensitive skin.
- Quality: Investing in a well-constructed mask from a reputable manufacturer may result in better durability, fit, and performance over time.
Adjusting Your CPAP Mask
Finding the most comfortable CPAP mask is only the first step—adjusting it properly is just as critical for comfort and effective therapy. Most commercial CPAP masks come in general sizes like small, medium, or large, but these categories don't always account for individual facial shapes, bone structure, or unique features like high cheekbones, narrow noses, or facial hair.
To achieve the best results, your mask should create a good seal without feeling overly tight or causing discomfort. A poor fit can lead to air leaks, skin irritation, or disrupted sleep—common reasons why people give up on CPAP therapy.
Many masks come with adjustable straps, headgear, or flexible cushions to help you personalize the fit. Some also offer optional accessories like mask liners, nasal pads, or chin straps to reduce leaks and improve stability. If you're experiencing discomfort or persistent leaks, don't hesitate to reach out to your sleep specialist or equipment provider. They can walk you through fine-tuning your mask or suggest a better-fitting option based on your needs.
Remember, a properly fitted CPAP mask should feel secure but gentle—supporting your sleep, not interrupting it.
Frequently Asked Questions
Using a nasal CPAP mask as a mouth breather can lead to reduced therapy effectiveness due to air leaking out of the mouth. However, mouth breathers can still use nasal masks if they wear a chin strap to help keep the mouth closed during sleep. Alternatively, a full-face mask may be a more reliable solution for consistent pressure delivery.
Nasal pillow masks are often considered the easiest to get used to, especially for new users. Their minimal design and lightweight fit reduce facial contact and pressure points, making them more comfortable for people who feel claustrophobic or sensitive to bulkier masks.
However, comfort is subjective, and the “easiest” mask will vary depending on your breathing habits and sleeping position.
Side sleeping is generally considered the best position for people using CPAP therapy. It helps keep the airway open and can reduce the risk of mask leaks compared to back sleeping, which may worsen airway collapse.
For those who prefer sleeping on their back, using a CPAP pillow or wedge can improve alignment and reduce obstruction. Stomach sleeping is less common but can work with low-profile masks like nasal pillows.
References
The information included on this site is for educational purposes only. It is not intended nor implied to be a substitute for professional medical advice. Contact your physician or health care provider when you have health related questions. Never disregard or delay medical advice because of information you have obtained on this site.