Aerophagia, or swallowing air, is one potential side effect of continuous positive airway pressure (CPAP) therapy. While some amount of aerophagia is normal, the stream of air that flows into the upper airway from a CPAP device can lead to a bothersome buildup of gas in the stomach and intestines.
If you use a CPAP machine, it might help to learn about aerophagia, including how it may be related to CPAP therapy and approaches for preventing and reducing the discomfort that it can cause.
What Is Aerophagia?
Aerophagia is the technical term that describes the swallowing of air. Everyone experiences small amounts of aerophagia throughout the day, including when eating and drinking. Aerophagia is the main way that gas enters the stomach.
What Causes Aerophagia?
Aerophagia can be caused by anything that prompts you to swallow air. It is normal for aerophagia to occur when swallowing saliva, drinking, or eating.
Increased amounts of air swallowing can be caused by CPAP therapy and may also occur due to other reasons, including:
- Eating or drinking quickly
- Chewing gum
- Experiencing anxiety and stress
- Smoking
- Being nauseous
- Lying on your back
- Using certain medications or drugs
Is Aerophagia Harmful?
Minor aerophagia occurs any time we swallow, and it is generally not harmful for a small amount of air to enter the stomach. Most of this air is removed from the stomach by belching, which keeps too much air from getting into the small intestine.
If excess gas builds up in the stomach or enters the small intestine, though, it may cause bothersome amounts of belching or flatulence. Significant aerophagia may also contribute to feeling bloated and other gastrointestinal symptoms.
Symptoms of Excess Aerophagia
Air swallowing is the main source of gas in the stomach. When too much aerophagia occurs, it can lead to an unwanted buildup of gas in the gastrointestinal system. This has the the potential to trigger a number of symptoms, including:
- Increased belching or flatulence
- Bloating
- Diarrhea
- Loss of appetite
- Stomach rumbling
It is important to note that these symptoms can be caused by many issues besides aerophagia. For example, other health conditions can heighten the production or gas in the gastrointestinal system.
Even when the amount of gas increases, it doesn’t always cause noticeable effects. In fact, many people with bloating and similar symptoms don’t actually have a significant buildup of intestinal gas. Instead, certain people might be more sensitive to gas, making them more likely to have symptoms even when the levels of gas in their gastrointestinal system are normal.
How Is Aerophagia Diagnosed?
To determine if a person has aerophagia, a doctor reviews their symptoms and overall health. The doctor will ask questions that help them understand the potential causes of gastrointestinal distress and may do some initial laboratory tests.
Extensive medical testing is usually not necessary unless a person has more severe symptoms that could be caused by an underlying gastrointestinal disorder.
How Do CPAP Machines Cause Aerophagia?
Using a CPAP machine can cause aerophagia because of the steady stream of pressurized air that the device pumps into the airway.
CPAP therapy is frequently used to treat obstructive sleep apnea (OSA), which is the most common type of sleep apnea. OSA involves frequent reductions or pauses in breathing during sleep. These changes in breathing are due to a blockage of the airway by tissues in the mouth and throat.
A CPAP machine sends a constant stream of pressurized air into the airway through a mask, which keeps the airway open. People using a CPAP machine can end up swallowing more air than usual because muscles in the esophagus relax during sleep, which can allow air from the CPAP to be pushed into the stomach.
Overall, it is estimated that around 16% of people using a CPAP have aerophagia related to the device. Both adults and children experience increased air swallowing during CPAP therapy.
Aerophagia causes some CPAP users to have issues with flatulence, belching, and feeling bloated. If these symptoms become significant, they may cause someone to reduce or stop the use of their CPAP machine. For this reason, it is important to address aerophagia in order to maintain the benefits of CPAP as a treatment for sleep apnea.
Preventing or Treating Aerophagia When Using a CPAP Machine
There is limited research about the best ways to prevent and treat aerophagia in CPAP machine users, but several different approaches may help.
A first step for anyone with symptoms of aerophagia is to talk with their doctor. Raising concerns about CPAP side effects early in the process may enable modifications to the device or mask settings to resolve these difficulties.
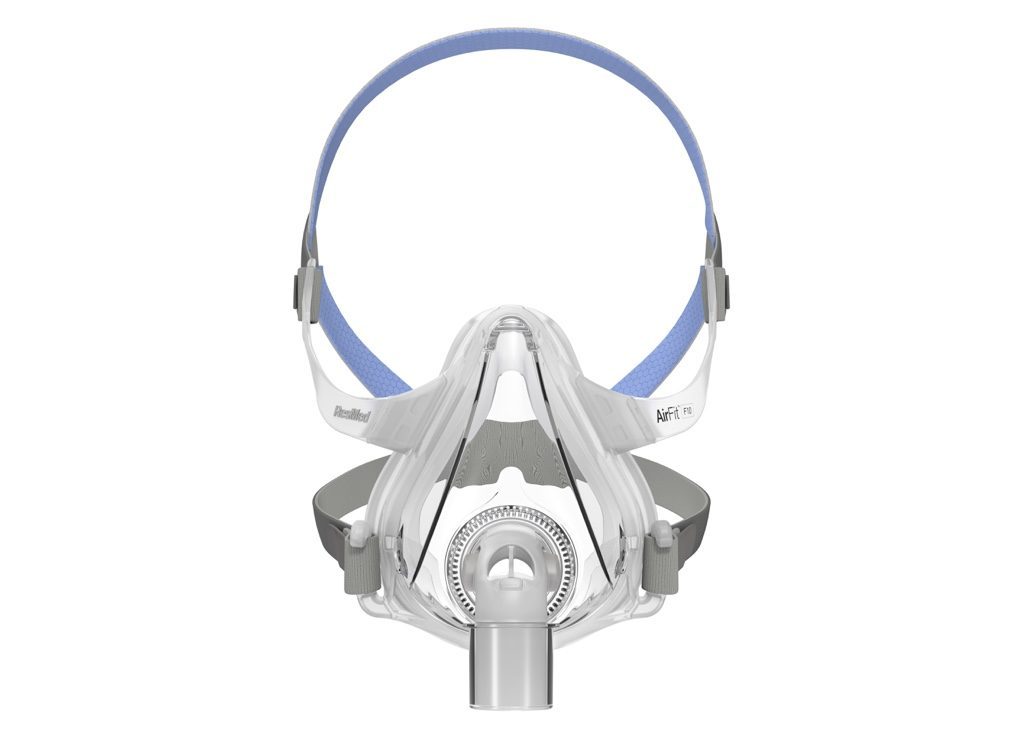
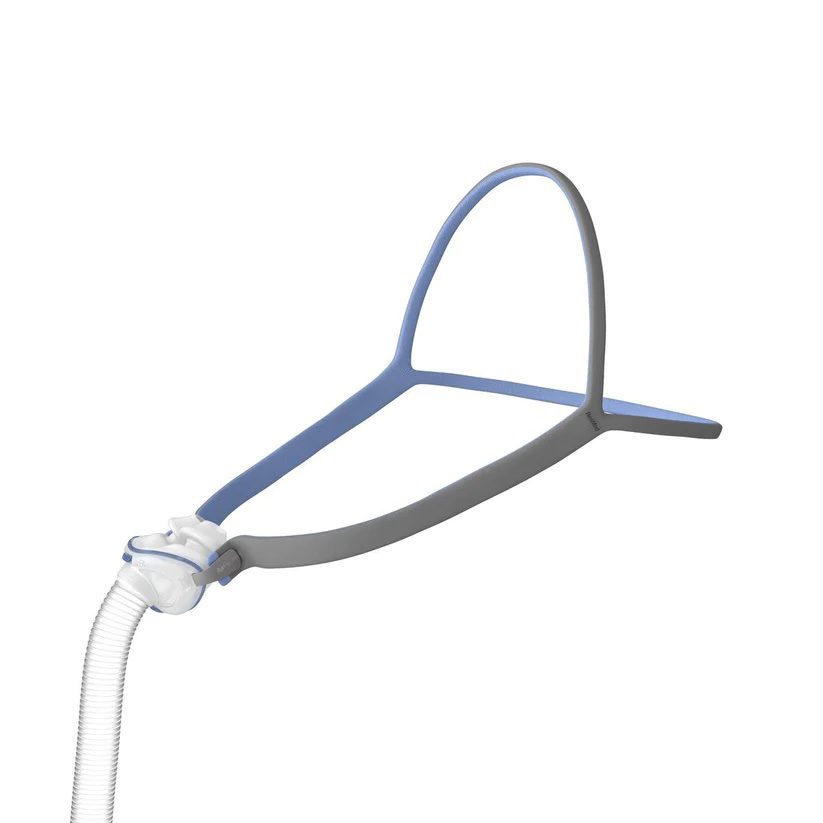
Changing the CPAP Mask
Although studies comparing mask types is limited, some evidence indicates that a nasal mask may cause less air swallowing than a full-face mask that goes over both the nose and mouth. When using a nasal mask, wearing a chin strap to keep the mouth closed may also reduce aerophagia.
People with a full-face mask should work with their doctor to make sure that it forms a tight seal on their face. Without a good seal, the CPAP machine may be set to deliver air at a higher pressure than needed, which may contribute to swallowing excessive air.
Reducing CPAP Pressure Levels
In some cases, your doctor may suggest trying to reduce aerophagia by lowering the pressure that is being pumped by the CPAP machine. The drawback to this approach is that if the air pressure is too low, the CPAP machine will not effectively treat sleep apnea.
For this reason, any adjustments to CPAP pressure levels should always be done carefully and under the guidance of a doctor or sleep specialist.
Trying a Different Kind of PAP Device
A CPAP is just one kind of positive airway pressure (PAP) device, and trying another PAP option may reduce aerophagia.
A small study found that an auto-adjusting positive airway pressure (APAP) device may cause less aerophagia than a CPAP. An APAP machine uses built-in sensors to monitor breathing and modifies the air pressure level accordingly. In this way, an APAP machine can provide reduced air pressure when a person is not experiencing breathing disruptions.
Through its ability to make these adjustments, an APAP device may decrease the average pressure over the course of the night and limit aerophagia.
Switching Sleeping Position
When using a CPAP machine, sleeping on your side instead of your back may decrease aerophagia. Sleeping on your side may also reduce the pressure level needed to keep your airway open when using an APAP machine, reducing bloating caused by air swallowing. As an added benefit, sleeping on your side is widely considered to help reduce the airway blockages that characterize obstructive sleep apnea.
Taking Anti-Gas Medications
Several brands of over-the-counter medications are designed to reduce the symptoms of intestinal gas. Although the intention of these medications is to break up gas bubbles, it has not been clearly proven that these medications relieve gas-related symptoms.
People with CPAP-related aerophagia who want to try these medications should talk with their doctor or a pharmacist for specific guidance. In most cases, the medication is taken before going to bed or during any nighttime awakenings that involve symptoms of excess gas.
Taking Other Steps to Reduce Intestinal Gas
While not specifically designed to address CPAP-related aerophagia, various practical steps may cut down on the buildup of intestinal gas. In most cases, this involves different methods for reducing air swallowing.
- Making dietary changes: What you eat can affect how much gas is produced in your gastrointestinal system. While the optimal diet varies from person to person, it is best to avoid any foods that trigger excess gas, which may include some vegetables like turnips and cabbage, dairy products, and certain artificial sweeteners.
- Limiting carbonated drinks: Aerophagia often increases from drinking carbonated beverages, so limiting these may help with symptoms of excess intestinal gas.
- Finding stress relief: Being stressed out can lead to more air swallowing, and symptoms like belching may worsen with stress and anxiety. Finding ways to relax may be beneficial, and you may find aromatherapy with certain essential oils to help with gas-related discomfort.
- Stopping smoking: Smoking increases air swallowing, so reducing or quitting smoking may help decrease excess intestinal gas.
- Avoiding gum: Because chewing gum can increase the amount of air that you swallow, it is often suggested to avoid gum to reduce bloating.
When to Talk to A Doctor
It is important to talk to a doctor if the symptoms of aerophagia are making it hard to use a CPAP device every time you sleep.
In most cases, aerophagia is normal and not a problem. However, swallowing too much air may cause uncomfortable symptoms. You should consult a doctor if you have significant bloating, belching, or flatulence and any of the following symptoms:
- Pressure or pain in your chest
- Blood in your stool
- Vomiting
- Diarrhea
- Worsening heartburn
- Pain in the abdomen
- Weight loss
Other Treatments for Sleep Apnea
Using a CPAP machine is not the only way to treat sleep apnea. For people who struggle with PAP devices, other types of treatment may be available.
For obstructive sleep apnea, there are several potential treatment options besides using a CPAP or other PAP machine.
- Lifestyle changes: Modifying certain habits and routines may significantly reduce breathing disruptions during sleep. Examples of changes that may be recommended include losing excess weight, getting regular exercise, avoiding sleeping on your back, and staying away from alcohol and certain drugs.
- Oral appliances: These devices are worn in the mouth during sleep and hold the tongue or jaw in a position that helps keep the upper airway open. Oral appliances are obtained with a prescription and are usually custom-fitted by a dentist.
- Implantable nerve stimulation: Often referred to by the brand name Inspire, this treatment involves implanting a small device in the chest. The device can monitor breathing and use a small pulse of electricity to stimulate the nerves that control muscles of the upper airway.
- Surgery: In some situations, surgery may be used to treat OSA by removing or repositioning the tissues in the mouth or throat that can block the airway.
For a less common type of sleep apnea called central sleep apnea (CSA), treatment is typically focused on addressing the underlying health condition causing irregular breathing during sleep.
Besides CPAP devices, treatment for CSA may include more technologically advanced forms of PAP therapy including certain types of bilevel positive airway pressure (BiPAP or BPAP) and adaptive servo-ventilation (ASV) devices.